Large Epiphrenic Esophageal Diverticulum with Achalasia
Progressive dysphagia in a 57 year old male • Xray of the Week
This 57-year old male presented with a 4-year history of progressive dysphagia with both solid foods and and liquids. CT scan of the chest with contrast and barium esophagogram were performed. What is the diagnosis?

Figure 1. CT scan of the chest with IV contrast. A. Axial image. B. Coronal image. What is the diagnosis?

Figure 2. Annotated CT scan of the chest with IV contrast. A. Axial image demonstrates a large outpouching (red arrow) with an air fluid level, due to the large esophageal diverticulum. B. Coronal image clearly shows the large right-sided esophageal diverticulum (red arrow) which communicates with the esophagus (green arrow). The esophagus is also dilated (yellow arrow).
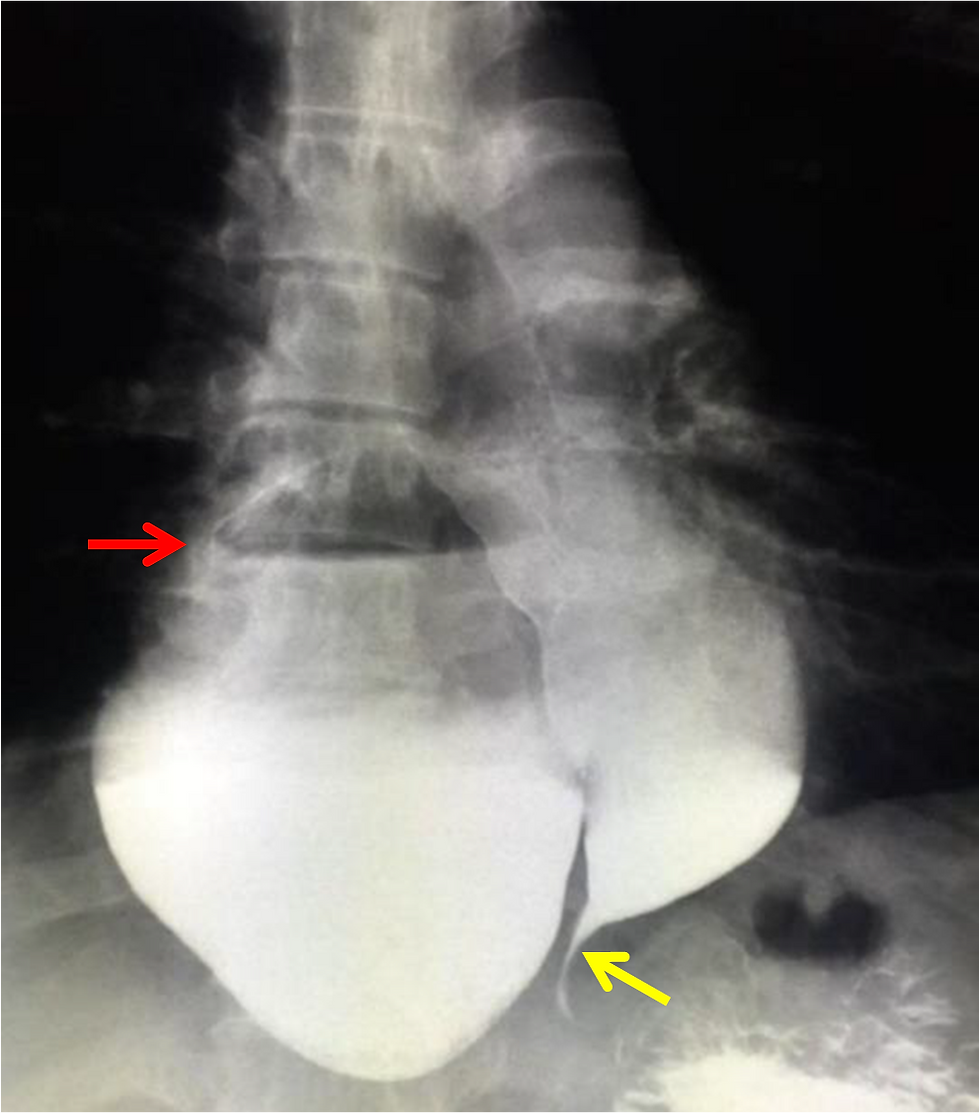
Figure 3. Esophagram depicts the presence of a large right-sided diverticulum (red arrow) approximately 8 cm from the gastroesophageal junction. There is pooling of the contrast inside the diverticulum as it communicates with the esophagus. The esophagus is also dilated with a characteristic “bird’s beak appearance”/tapering (yellow arrow) near the gastroesophageal junction.
Discussion:
Epiphrenic esophageal diverticulum (EED) is an uncommon form of esophageal diverticulum with an incidence of only 1:500,000/year in the adult population, and comprises about 10% of all esophageal diverticula. Arising in the distal esophagus, it is typically located 4 to 8 cm above the cardia or in the last 10 cm of the esophagus (1-3). It is a pulsion type of diverticulum caused by motility disorders with markedly increased intraluminal esophageal pressures (1-2). Presentation in infants and children is rarely seen (4). In addition to other motility disorders, achalasia is almost always associated with EED (5). Achalasia itself is a rare entity with an approximate incidence of 1:100,000 people/year (6-7). Clinical manifestations of EED are variable but most commonly include dysphagia and regurgitation which usually progress over time (8). However, up to eighty percent of patients may be asymptomatic. Diagnosis is usually made via barium swallow with supplemental evaluation including upper endoscopy to exclude malignancy and esophageal manometry to delineate any underlying motility disorder (9). Treatment strategies, either open or laparoscopic surgery, involve esophageal myotomy, diverticulectomy and fundoplication. Myotomy decreases the incidence of diverticulum recurrence and partial fundoplication has been proposed as the most appropriate anti-reflux method. Surgery appears to be an effective treatment but is associated with significant mortality and morbidity, thus is it reserved for patients with symptomatic EED (10).
References:
1. Debas HT, Payne WS, Cameron AJ, et al (1980). Physiopathology of lower esophageal diverticulum and its implications for treatment. Surg Gynecol Obstet; 151:593–600. 2. Dodds WJ, Stef JJ, Hogan WJ, et al (1975). Radial distribution of peristaltic pressure in normal subjects and patients with esophageal diverticulum. Gastroenterology; 69:584–590. 3. Clouse RE, Diamant NE (2006). From Esophageal motor and sensory function and motor disorders of the esophagus. Sleisenger and Fordtran’s Gastrointestinal and Liver disease. Edited by Feldman M, Freeman LS, Brandt LJ. Philadelphia, WB Saunders; 855-904. 4. Zaninotto G, Portale G, Costantini M, et al (2011). Therapeutic strategies for epiphrenic diverticula: Systematic review. World J Surg; 35:1447-53. 5. Fisichella PM, Jalilvand A, Dobrowolsky A (2015). Achalasia and epiphrenic diverticulum. World J Surg.; 39 (7):1614-9. 6. Vaezi MF, Richter JE (1999). Diagnosis and management of achalasia. American College of Gastroenterology Practice Parameter Committee. Am J Gastroenterol; 94: 3406 – 12. 7. Francis DL, Katzka DA (2010). Achalasia: update on the disease and its treatment. Gastroenterology; 139: 369 – 74. 8. Thomas ML, Anthony A, Fosh BG, et al (2001). Esophageal diverticula. Br J Surg; 88: 629-42. 9. Fasano NC, Levine MS, Rubesin SE, et aI (2003). Epiphrenic diverticulum: clinical and radiographic findings in 27 patients. Dysphagia; 18 (1):9e15. 10. Benacci JC, Deschamps C, Trastek VF, et al (1993). Epiphrenic diverticulum: results of surgical treatment. Ann Thorac Surg; 55:1109 –1114.

Karl John A. Koa, MD completed his Doctor of Medicine at West Visayas State University, in La Paz, Iloilo City, Philippines. He is currently the senior and Chief Resident Physician in the Department of Radiology at Chong Hua Hospital, also in Philippines. He has presented case reports in the West Visayas State University including a case report contest on Neurofibromatosis Type 2, which he won last 2015 during his post graduate internship training.













Comments